How to prescribe medicinal cannabis in Australia
This article was reviewed by Dr Jim Connell a GP and medicinal cannabis prescriber. This information is for educational purposes only and is not medical advice.
This article aims to be the go-to resource for any healthcare practitioner who wants to learn how to prescribe medicinal cannabis in Australia. It will teach you the process of prescribing and be your guide to everything you need to know to be a successful prescriber of medicinal cannabis.
Medicinal cannabis has been legal Australia-wide since 2016. There are about 80k legally prescribed medicinal cannabis patients in Australia, with many patients self-medicating. As of December 2021, cannabis has been prescribed for over 100 medical conditions. Unfortunately, many healthcare practitioners cite lack of evidence as the reason that they don’t want to add medicinal cannabis to their treatment plans. However, there is ample real-world evidence and a growing volume of clinical evidence for medicinal cannabis.
Across the globe, cannabis medicine has been patient-driven. Here in Australia, patient uptake of cannabis medicine is increasing rapidly. As a modern healthcare practitioner, you must learn about medicinal cannabis, the potential benefits and the limited side effect profile.
If your concern is not about cannabis itself but about prescribing medicinal cannabis, don’t worry. It’s straightforward. If you are still on the fence for any reason, here are some interesting facts that might get you across the line:
- Any GP or specialist Australia-wide can prescribe medicinal cannabis, and you do not need a license to prescribe.
- The Therapeutic Goods Administration (TGA) requires clinical justification for scripts which means the TGA believes cannabis is helpful as a medicine.
- The top conditions for which medicinal cannabis is approved are: Chronic Pain, Anxiety, Cancer Pain, Insomnia, Neuropathic Pain & PTSD.
- There is evidence that cannabis works – limited clinical evidence and a lot of real-world evidence.
- There are products available to patients that have been in clinical trials.
- Cannabis has been proven to reduce pain in chronic pain patients by about 30%.
- While some cannabis medicine is expensive, there is a vast range of products which means you’ll find suitable products for most patients.
It’s important to note that this is an overview of what you need to know. We’ll expand upon these concepts in articles listed in each section’s “Further Reading” resources, some of which are in progress and not available yet.
Below is everything we’ll cover in this article. If you want a quick overview, we recommend you read the sections with the asterisks next to them:
- Getting started
- Cannabis 101
- Patient considerations
- Suitability and eligibility for treatment
- Prescribing cannabis to a self-medicating patient – Coming Soon
- Cannabis/CBD Contraindications and interactions with other drugs**
- The importance of listening to your patients (who have cannabis knowledge) – Coming Soon
- Suitability and eligibility for treatment
- Understanding products
- Medicinal cannabis preparations & delivery methods – Coming Soon
- How to choose a medicinal cannabis product for your patient – Coming Soon
- Dosages and titration – Coming Soon
- Prescribing cannabis medicine
- Pathways: Special Access Scheme (SAS) & Authorised Prescribers (AP)*
- SAS Application and AP reporting – Coming Soon
- How to run a medicinal cannabis consult **
- Patient management plan and follow up schedule – Coming Soon
- Pathways: Special Access Scheme (SAS) & Authorised Prescribers (AP)*
- After the script
- Dispensing medicinal cannabis (Pharmacies) – Coming Soon
- Best practices for patient follow up and monitoring
- Conclusion
Who can prescribe medicinal cannabis in Australia?
Any GP or Specialist can prescribe medicinal cannabis Australia-wide and depending on the jurisdiction, Nurse Practitioners may also be eligible to prescribe cannabis. Each state and territory has slightly different rules about prescribing. Some states require an application to both the TGA and state health department; others have more streamlined processes. If you’re not comfortable prescribing medicinal cannabis and would like to see how it might help a patient before writing your first script, you can always send your patient to a cannabis clinic. It’s essential to contact the clinic to get your patient’s results.
Further Reading:
- Who can prescribe medicinal cannabis by Dr Jim and Nurse Cam – Coming Soon
How does cannabis work?
Cannabis works by interacting with a natural system that we already have in our bodies, our Endocannabinoid systems.
The Endocannabinoid System
The human body has a biological system called the Endocannabinoid System (ECS). The ECS is responsible for maintaining homeostasis, is known to regulate various bodily functions that are critical for health and wellbeing and plays an essential role in our central nervous system and immune systems. The ECS is made up of three two main parts:
- Cannabinoid receptors
- Cannabinoids
- Enzymes that break down the cannabinoids
Cannabinoid receptors are located throughout the nervous and immune systems. There are two main cannabinoid receptors – CB1 and CB2. When activated, these receptors are responsible for increasing or decreasing nerve signalling.
Endocannabinoids and phytocannabinoids may also interact with other receptors to exert their effects. Some of those receptors include: GPR55, TRPV1, PPAR, GPR119, GPR18.
There are three types of cannabinoids:
- Endocannabinoids – endogenous cannabinoids which your body makes naturally.
- Phytocannabinoids – plant cannabinoids found in plants.
- Synthetic cannabinoids – human made cannabinoids
Phytocannabinoids and synthetic cannabinoids have similar chemical structures to our endocannabinoids and can help moderate our internal system when ingested.
To simplify things, cannabinoids can work with the cannabinoid receptors like lock and key. The receptors are the locks, and the cannabinoids are the keys. Once engaged, the receptors set off processes to modify the nerve signals. CBD, THC and the other cannabinoids work on both cannabinoid receptors and various other receptors to help balance our bodily functions. Most minor cannabinoids interact with non-classical cannabinoid receptors, which we’ll discuss more in another article.
Further Reading:
- Watch Dr Matty Moore explain the Endocannabinoid System
Clinical Endocannabinoid Deficiency
Clinical Endocannabinoid Deficiency (CECD) is a hypothesis posed by Dr Ethan Russo in the early 2000s. It posits that deficiencies in Endocannabinoid levels are the root cause of many common diseases and health disorders that share a general set of characteristics. The thinking is that by up-regulating the ECS, you can reduce symptoms of these otherwise almost untreatable conditions. Over the last 20 years, research has begun to validate the existence of CECD.
CECD conditions include:
- Chronic migraines
- Irritable bowel syndrome
- Endometriosis
- Fibromyalgia
- Anxiety and depression
- PTSD
Unlike most conventional drugs, which focus on a single element of disease, cannabis, when used correctly, can shift an entire network of physiological systems through its interaction with the ECS. Our understanding of the exact processes behind most diseases is limited. Cannabis allows us to effect positive change without the same risk.
Further Reading:
- What is Clinical Endocannabinoid Deficiency (CECD) by Dr Jim & Nurse Cam – Coming Soon
Understanding: CBD vs THC
CBD and THC are the two best-known cannabinoids in the cannabis plant but have very different profiles.
CBD is a promiscuous molecule that acts through various receptors, enzymes and neurotransmitters within the body, giving it a wide range of clinical actions. Despite its effects across a broad range of systems, it is surprisingly well-tolerated and causes few severe side effects. CBD is known to reduce anxiety, inflammation and seizure rates in paediatric epilepsy.
It is so safe that the World Health Organisation publicly stated that CBD “Does not appear to have abuse potential or cause harm.” Some of the benefits that CBD is known for are:
- Reducing pain
- Increasing sleep
- Lessening anxiety and depression
- Decreasing nausea
- Improving heart health
- Revitalising and protecting skin
Side effects of CBD often dissipate after titration or are found at very high doses of CBD. Side effects include:
| Diarrhoea | Dry mouth |
| Vomiting | Drowsiness |
| Fatigue | Low blood pressure |
| Pyrexia (fever) | Lightheadedness |
| Somnolence (drowsiness) | Low appetite |
| Abnormal results on liver-function tests | Weight loss |
It’s also important to note that there is potential for drug to drug interaction through cytochrome P450 enzyme inhibition which you will learn more about below.
THC is the most abundant and pharmacologically active chemical in the cannabis plant. THC is known for the euphoria (high) that we often associate with adult-use (or recreational) cannabis consumption. However, with medicinal cannabis experiencing intoxication is often seen as an adverse event. THC can be a powerful medicine at low doses and exerts its effects through direct interactions with cannabinoid receptors.
THC doesn’t suppress the cardiorespiratory centres of the brain because there is a low density of cannabinoid receptors in the brainstem. Therefore, THC has an excellent safety profile. However, having too much THC can be a very unpleasant experience for patients.
THC is associated with most cannabis side effects; however, these can be mitigated with a low and slow titration or pairing with CBD to widen an individual’s therapeutic window. Side effects can include:
| Intoxication | Over-sedation |
| Headaches | Dizziness, unsteadiness or lightheadedness |
| Nausea | Insomnia |
| Anxiety or panic | Shaking |
| Palpitations | THC Dependence |
| Dry mouth | Memory loss |
Further Reading:
- CBD vs THC and combining cannabinoids by Dr Stephen Chalk – Coming Soon
Understanding terpenes
Terpenes are aromatic oils found in the leaves, flowers, fruit and sap of plants, including cannabis. Terpenes protect the plant and give the plant smell and flavour. Research has shown that terpenes have a range of medicinal properties; however, most of this is still pre-clinical.
In addition to being responsible for aromas, terpenes are considered the ‘effect drivers’ of cannabis chemovars. Many people think that the plant species, Indica or Sativa, dictates the product effect. However, it’s actually the terpenes.
Terpenes and cannabis products
Not all medicinal cannabis products contain terpenes. Full-spectrum products contain terpenes as they are an extraction of the full range of plant chemicals. However, it’s important to know that, even in a full spectrum extract, many compounds found in the plant are lost due to their volatile nature. As a result, even a full spectrum extract will likely have a different chemical profile to the original flower.
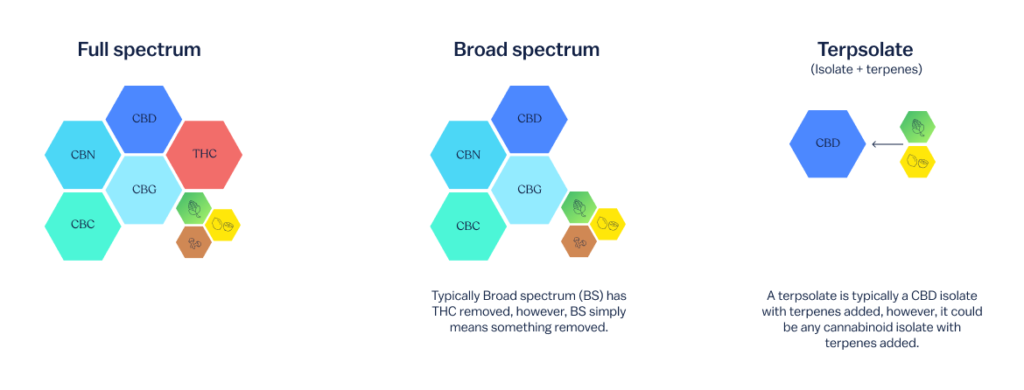
Broad-spectrum products should have terpenes. However, broad-spectrum means something has been removed from the full extraction.
Isolates are a single molecule and will not have terpenes. And, more recently some companies are creating terpsolates which are isolates with terpenes added.
Terpenes alone will not create the ‘high’ that can happen from THC; however, terpenes may be able to modulate the effects of THC.
Further Reading:
- Understanding Terpenes: Terpenes 101 by Dr Jim and Nurse Cam
- Common Terpenes: Their Benefits, Doses & Effects by Dr Jim and Nurse Cam
Evidence for medicinal cannabis
It’s almost impossible to write something that comprehensively summarises the evidence for medicinal cannabis because new research is published daily. While people often say there is not enough evidence for the use of medicinal cannabis, that is simply not true. There is limited double-blind placebo-controlled trial evidence for cannabis. This is because there are various unique challenges that natural medicines present.
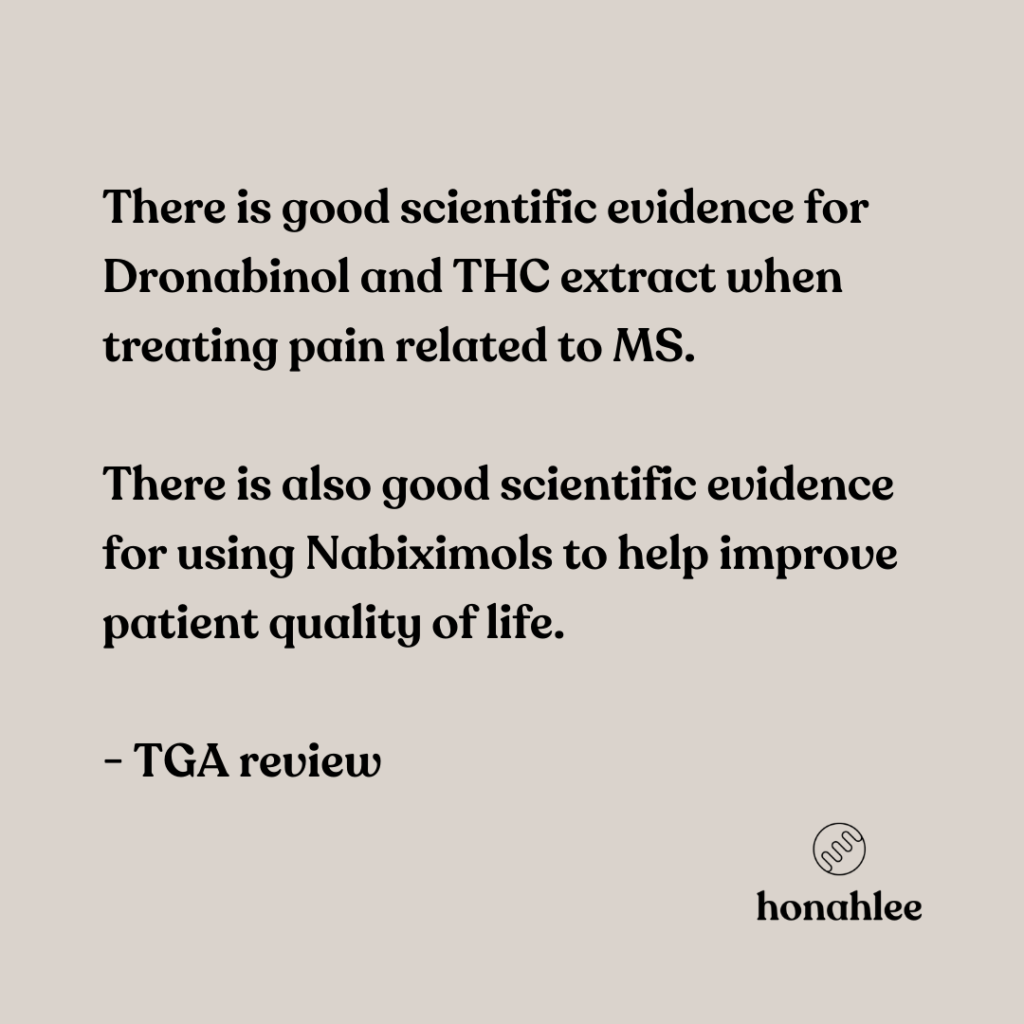
However, there is a growing body of evidence for both THC and CBD. Dronabinol, a THC based medication has been around since the 1980s and Sativex, a balanced THC:CBD product, is registered on the ARTG.
Finally, when looking at minor cannabinoids, the evidence becomes sparse.
Here is a snapshot of the evidence for the use and prescription of medicinal cannabis:
CBD:
- Supports seizure reduction in patients with Dravet and Lennox-Gastaut syndromes (Ref 1, Ref 2)
- Pain reduction – neuropathic pain (Ref 1, Ref 2)
- Improvements in sleep – 1:1 ratio CBD:THC (Ref 1)
THC:
- Reduction of nausea and vomiting (Ref 1, Ref 2)
- MS-related pain (Ref 1)
- Improvements in sleep (1:1 ratio) (Ref 1)
Further Reading:
- The scientific evidence for medicinal use of cannabis – Coming Soon
Benefits, side effects and risks of cannabis
Cannabis is often thought, incorrectly, to be a highly addictive drug that can cause psychosis. This idea that cannabis is inherently bad comes from cannabis prohibition and the limited clinical evidence for the medical use of cannabis. Cannabis consumption for any purpose does come with potential side effects. But, most of the research showing cannabis causing significant side effects is from studies performed on recreational populations who are not consuming cannabis correctly to achieve medical and health and wellness benefits.
When talking about the benefits and side effects of cannabis, we’ll focus on CBD and THC.
Some of the benefits that CBD is known for are:
| Analgesic | Antiemetics |
| Sedative | Improving heart health |
| Anxiolytic and antidepressant | Revitalising and protecting skin |
Side effects of CBD often dissipate after titration or are found at very high doses of CBD. Side effects include:
| Diarrhoea | Dry mouth |
| Abnormal results on liver-function tests (mostly related to drug-drug interactions)* | Drowsiness |
| Vomiting | Low blood pressure |
| Fatigue | Lightheadedness |
| Pyrexia (fever) | Low appetite |
| Somnolence (drowsiness) | Weight loss |
* There is some evidence that CBD is hepatoprotective.
Benefits of THC include:
| Sedative | Anxiolytic |
| Antiemetic | Relaxant |
| Analgesic | Anticonvulsant |
| Anti-Inflammatory | Appetite inducer |
| Antispasmodic – muscles and bowels | Antidepressant |
Side effects of THC can happen at lower doses but can often be mitigated by starting very low and increasing slowly. Side effects include:
| Headaches | Over-sedation |
| Nausea | Dizziness, unsteadiness or lightheadedness |
| Anxiety or panic | Insomnia |
| Palpitations | Shaking |
| Dry mouth |
Like all powerful medicines, cannabis may have side effects; however, this can be mitigated with appropriate dosing and monitoring. In comparison to other medications, cannabis can be a safe and well-tolerated alternative or adjunct. One of the main benefits of cannabis is that it works across a range of different physiological systems. As a result, cannabinoid therapy may minimise the side effect burden of poly-pharmacy.
Further Reading:
- Benefits and side effects of CBD oil
- Cannabis myths & facts – Coming Soon
Suitability and eligibility for treatment
The following criteria make a patient eligible for medicinal cannabis:
- The patient has a chronic condition (diagnosed for greater than three months) and
- Has been unresponsive to past treatment or experienced intolerable side effects from those treatments.
It’s important to note that past treatments may include:
- Prescribed medications or
- OTC treatments or
- Lifestyle, dietary and behavioural modifications
While medicinal cannabis is not a first-line treatment, it may be used as a second-line treatment. The TGA has approved medicinal cannabis for over 100 conditions to date. It’s not just for significant illnesses or end of life management.
Further Reading:
Cannabis Contraindications and Precautions
Cannabis is generally well tolerated and has limited side effects. Compared to other prescribed medications like opioids and antidepressants, cannabis has a much smaller side effect profile. A CBD isolate has an even smaller side effect profile. There are, however, some contraindications and circumstances where patients will need to be monitored when starting cannabinoid treatment. Here’s a list of things to consider when prescribing a patient cannabis.
Contraindications
| General (CBD & THC) | THC Specific |
|---|---|
| Allergy to cannabinoids or hemp oil | History of psychosis |
| Pregnant or breastfeeding | |
| Unstable cardiovascular disease |
Precautions
- Sensitivity to cannabinoids or hemp oil
- History of substance abuse
- Renal and hepatic impairment
- Cardiovascular disease risk factors
- Cancer immunotherapies
- Bipolar (can have an increase in rapid cycling with THC)
- Severe mental health issues
- Immunosuppression therapy (use of tacrolimus)
- Certain medication (see the cannabis drug interactions section below)
Cannabis Drug interactions:
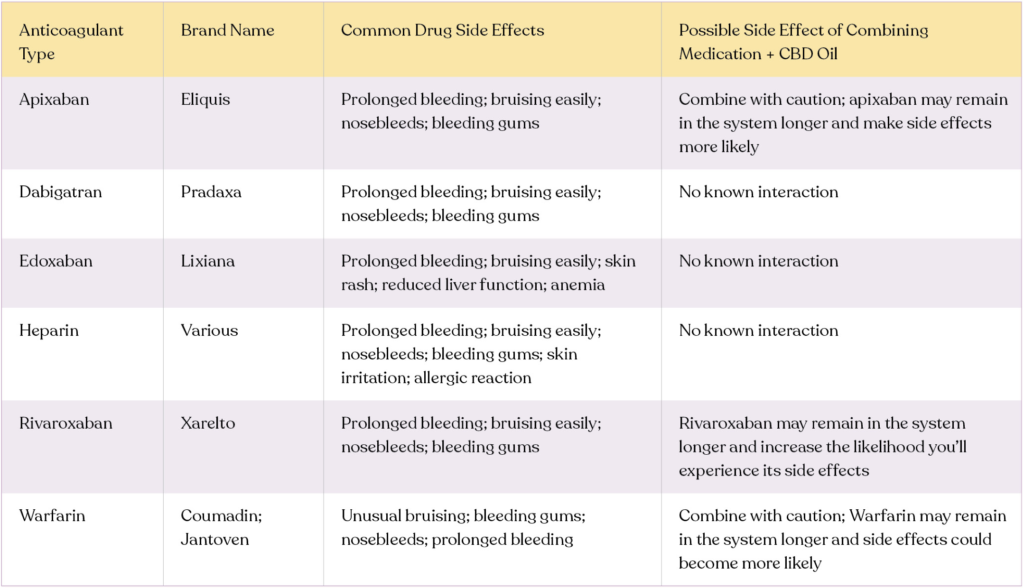
Both THC and CBD may interact with medications and may affect how the patient’s current medications work. Therefore, it’s critical that you understand a patient’s current medication regime. In addition, ongoing monitoring of medications may be required when starting medicinal cannabis.
The following is a list of the best-known cannabis and other drug interactions, most of which involve the Cytochrome P450 Enzymes.
Both CBD & THC:
- Drugs metabolised by the CYP3A4 and CYP2C9 pathways
CBD Only:
- Drugs metabolised by CYP2C19 and CYP2D6
THC Only
- Drugs that interact with CYP1A2
Further Reading:
- Cannabis contraindications & interactions with other drugs – Coming Soon
- CBD Benefits, side effects and drug interactions on honahlee.
Pathways: Special Access Scheme (SAS) & Authorised Prescribers (AP)
Any GP or Specialist can prescribe medicinal cannabis in Australia. In some jurisdictions, Nurse Practitioners may also prescribe. Because cannabis is an unapproved medicine, you must go through a special application pathway to get authorisation from the TGA to prescribe. There are two main pathways through which you may be given authorisation:
- Special Access Scheme B
- Authorised Prescriber Scheme
Special Access Scheme B (SAS B)
The SAS B application can be submitted in paper format; however, the preferred method is online via the SAS Portal. Through the portal, healthcare practitioners can fill in and submit an application to both the TGA and State Health Departments (where applicable). It’s important to note that in Tasmania, prescribers must submit their application to the local health department separately.
The application consists of patient details and medical history, a prescriber justification, product category selection, and a high-level treatment plan. The application takes between 5-10 minutes once you’ve become accustomed to the platform. Because you’re applying to prescribe a category of medicines, once approved, you can select any product in that TGA category. If you and your patient decide they’d like to test a different product in that same category, or the original product is out of stock, you may simply write a script for that product without re-applying.
While experienced prescribers use the SAS B, most prescribers who see patients regularly prefer the Authorised Prescriber pathway.
Authorised Prescriber Scheme (AP)
The AP pathway is for more experienced prescribers. Any GP or specialist may become an AP. However, Nurse Practitioners are not eligible to become APs.
To become an AP, a prescriber must undertake an extensive application process. Product suppliers will often complete and submit the AP application for prescribers. There are two types of AP applications:
- Standard pathway
- Established history of use pathway
The Standard Pathway for APs is a two-step process.
- Step 1: is to get approval from a human research ethics committee (HREC) or endorsement by a specialist college.
- Step 2: Once you have this approval, you may apply to the TGA.
Application to the TGA is an application for a specific category of products. Once approved to prescribe that category of products, you may prescribe any product in that category to patients without re-applying for each product.
Established history of use pathway
This pathway only requires an application to the TGA; you do not need any other approval. When applying for this authorisation, you may only apply for a special category of products deemed to have an established history of use. The established history of use products are broken into three categories and consist of:
- Liquids and capsules that are
- CBD dominant or balanced (CBD & THC) products for
- Chronic pain and anxiety in adult patients
Once approved, you may prescribe any product that falls into one of the three categories for the conditions specified in the list above.
Further reading:
- An in-depth look at the SAS and AP Pathways – Coming Soon
- A step by step walkthrough (tips and tricks) of the SAS Portal – Coming Soon
How to run a cannabis consultation
Running a medicinal cannabis consultation isn’t much different from any other medical consultation. Your goal is to understand the patient’s circumstances, condition and then derive the right treatment plan to help improve the patient’s health and overall wellbeing. The consultation is the core part of the medicinal cannabis process. The information below is written to show you how similar a cannabis consultation is to a typical consultation. If you’d like to see an in-depth overview of how to run a consultation, please review the further reading resources below.
Understanding the condition and symptom severity
You will do the same diagnostic workup you’d do if you were planning to prescribe any other medication to treat the condition. The goal is to find out what’s going on, what needs timely intervention and what symptoms medicinal cannabis might help manage in the longer term.
You must be able to identify the primary condition and any sort of secondary conditions or symptomatology. For example, it’s common for an individual with chronic pain to have difficulty sleeping. When doing this assessment, keep Looking for ECS dysfunction, which is most easily identifiable in homeostatic dysfunctions, in the back of your mind. Knowing what the primary condition and symptoms are as well as the secondary symptoms will allow you and the patient to work together to manage expectations and narrow down treatment goals.
Identifying contraindications and precautions (patient history)
There is a limited range of cannabis contraindications and drug interactions as listed above. While cannabis is relatively safe compared to conventional medications, it’s important that you know and take these considerations into account. To review the contraindications and drug interactions, please scroll up. Some of the other considerations include:
- Suspected or confirmed family history of mental illness
- Suspected or confirmed personal history with mental illness, specifically schizophrenia
- A history of or current drug use disorders
- Past drug or alcohol abusive (addictive personalities)
- Smoking history – tobacco and cannabis
- Cardiovascular disease
- History of psychosis or mental illness
- Current medications and supplements – may need to monitor.
Further Reading:
- Cannabis/CBD Contraindications and interactions with other drugs – Coming Soon
Current and past use of cannabis
Many medicinal cannabis patients have tried cannabis in the past or maybe self-medicating. You must encourage your patient to tell you about their experience with cannabis as it will give you some indication of how they’ve reacted and any sort of tolerance to the medication they may have. Patients will often be wary about talking about historical cannabis consumption with their doctor.
A patient’s past or current cannabis consumption may also impact the product you start the patient on and treatment goals. For example, a patient who self-medicates with THC will likely need to start with a prescribed medication containing some THC. Suppose a patient is currently using cannabis from the green market (illicit market) or smokes to relieve symptoms. In that case, you may decide that removing illicit cannabis and moving from smoking to vaping are two aspects of the treatment goals.
Patient expectations & goal setting
Patient knowledge or perceived knowledge of what medicinal cannabis can do varies greatly. Patients who have frequently used cannabis in the past may know a lot about cannabis. In some cases, they may know more than you do. Therefore, while making sure you are still responsible for leading the patient’s treatment, you may also be able to use the experience patient as a learning experience.
Patients who have not consumed cannabis in the past will have varying concerns; however, both experienced consumers and cannabis naive patients must know that cannabis is not a panacea. Like all other medications, cannabis may work well for some and not for other patients. The main goal of expectation setting with a patient is to answer the question:
“What does being unencumbered by your condition look like to you?”
Once you as a healthcare practitioner understand this, you’ll manage both patient expectations and your treatment plan even better. As with other conventional medications, ideally, you can reduce symptoms and manage the condition. However, for some patients, a primary goal may be to get them active again or improve their overall quality of life.
Product selection
Remember that while cannabis alone can help manage symptoms for some patients, it’s often used in conjunction with other treatments. For some patients, cannabis may help reduce their current burden of poly-pharmacy or mean they no longer need to take other medications, while for others, it may not work at all.
Product selection can be a very tricky part of medicinal cannabis. The perceived difficulty of authorisation to prescribe (access pathways) and the drug driving laws are two factors that immediately create a bias in product selection. While those factors must be considered, the patient and providing genuinely patient-centred care must be the determining factors of treatment.
The condition and symptoms you aim to treat should be the number one factor. Cannabis works differently for everyone. Other factors to take into account are:
- Chronicity of the condition
- Duration and frequency of flare-ups
- Variable that exacerbate the symptoms
- Past experiences
- Patient product knowledge
- Lifestyle and circumstances (cost, driving, workplace drug testing, operation of heavy machinery etc.)
Once you have a clear picture of these factors, you can choose a product. While there are some rough guides on the type of product you may want to prescribe for specific patient profiles, there are no hard and fast rules.
There are over 300 products available for patients, and they can be tough to differentiate. It’s important to point out that many patients already know about the products available and what’s in them. There’s no way that you can be expected to know about all of them. However, you must have the resources and knowledge to learn about a new product if your patient asks for it. Product suppliers can be a great resource to learn more about products. But tools like Catalyst bring all the product information together to allow you to do quick on the spot learning and comparisons between products. These tools can help empower you to lead the treatment plan and give your patients the confidence that you’re open to listening to them and putting them at the centre of their treatment.
Dosing and titration
The general rule for dosing and titration of medicinal cannabis is “start low and go slow”. Cannabis is a unique treatment because it does work quite differently from person to person. Patients must be mindful of how cannabis makes them feel and reflect on changes in their symptomology. At first, even small changes are a positive sign. These changes or improvements should increase as the patient titrates up.
It’s important to remember that CBD and THC have different effects and when consuming THC, patients may notice effects more quickly than with CBD. The goal is to find the optimal therapeutic window, which is where the patient gets the most benefit without unwanted side effects.
Titration duration varies and will depend on patient factors that you’ve uncovered in the consultation process as well as the product selected. For example, flower titration is very different to titration with an oil. Some patients might be comfortable titrating a bit faster, and some may want to take it more slowly. You’ll work with the patient to find a balance and provide them with education and materials that will help them determine their therapeutic window.
By the end of your consultation, both you and the patient should feel like you’re on the same page with expectations and goals. But, even more important is that the patient feels optimistic about the treatment plant and confident in starting their medicinal cannabis regime.
Further Reading:
- How to run a cannabis consultation by Dr Jim and Nurse Cam – Coming Soon
Best practices for patient follow up and monitoring
For a patient to see the best benefits from medicinal cannabis, they should be taking their medication and be making lifestyle changes to up-regulate their Endocannabinoid Systems. The main reasons patients don’t see benefit from cannabinoid treatment are
- Incorrect product selection
- Inappropriate dosing and titration
- Lack of patient compliance to the treatment plan
- Underlying symptoms have unknown aetiology and require appropriate diagnostic work up before commencing treatment. There may be a more definitive or appropriate treatment available.
Patient follow-up and monitoring are key to getting the best outcomes for your patients. Making follow up and compliance easy starts in the initial consultation. Here are some tips to help you get the best out of your patients:
Explain your process
Particularly for cannabis naive patients, you mustn’t give them too many repeats. Explain why you’re giving the repeats you are and how often you expect to have follow-ups at the start. Discuss any adverse events and what they can expect. If you’re monitoring other medication-blood levels, be clear about why and how often. And, if a patient is aiming to reduce other medications or illicit cannabis consumption, make sure you’ve spoken with them about down-titration and a schedule. Again, the patient must know what to expect.
Be clear about dosage and titration
Be clear with the patient about the difference and relationship between mg and mL and how they relate to the product you’ve prescribed. Because patients can get anxious and excited about the potential of symptom relief, make sure the patient is willing to titrate up slowly and mindfully.
Patients must track symptom changes and effects
Particularly when searching for the optimal dose, it’s essential that patients track their symptoms pre and post administration and log any adverse events that may occur (even if they are minor).
Stay goal-oriented
A patient may not see benefits immediately or at all. It can take up to 4 weeks for a patient to notice the full benefits of CBD, whereas THC has more immediate feedback. A patient may find that specific symptoms are reduced, but others are not. Make sure that you’re focused on the individual parts of the overall plan, not just one big win.
If a patient says cannabis isn’t working, listen
Everyone responds differently. You must understand what the patient means by ‘it isn’t working. If there are side effects, consider interactions with other medications and other potential contributing factors. Perhaps the patient has gone past their optimal dose, or there have been changes in other aspects of their care? Because cannabis is such a unique experience for each patient, it’s important you understand the context of a patient’s comments.
Map the follow-up schedule
Reviews are more frequent in the initial stages of treatment to fine-tune product selection and dose and monitor for adverse effects or problematic use. These may be 2-4 weekly if required.
Once you’ve established dosage and products and the patient is confident with their regimen, reviews may become less frequent. Potentially move to every few months.
Ongoing appointments are to monitor progress, assess goals, change products (if required), assess for tolerance, side effects or problematic use.
Note: If a patient’s health status changes due to the evolution of their condition, they may need more frequent monitoring to help them through these changes.
Conclusion
While it may seem like there is a lot to know about prescribing medicinal cannabis, once you’ve trialled it with a few patients and understand the process, it’s very straightforward. For many patients, cannabis has completely changed their quality of life for the better. So whether you decide to become a regular prescriber of medicinal cannabis or use it with your patients as a last resort, it can be a valuable part of your medical toolkit.